2500 years ago, the Greek philosopher Parmenides said, “Give me the power to cause fever, and I’ll cure all disease.”
That’s right – the ancients recognized inflammation as a medical phenomenon long ago. They even theorized that medically induced fever might be an effective treatment for mental disorder. So, paradoxically, if inflammation can cause mental unrest, then fever might be able to relieve it.
Fever is a kind of acute inflammation, induced by infection. The body raises its core temperature to make invading pathogens leave it. That’s turning up the heat to our benefit. So, running a fever is actually a good thing. It means the body’s fighting to live.
But, as we’ve discussed in our past few blogposts, there’s a downside to body heat, especially when it burns out of control. We now know that inflammation is the key ingredient in causing chronic disease. And, in the case of autoimmunity, inflammation is the root cause. However, we’re just beginning to understand the many aspects of this phenomenon, one of which is pain.
How the Body Communicates Pain
Pain is a key component of inflammation. After all, fire burns! The body communicates the sensation and awareness of pain, to and from the brain, via two intricately connected systems:
- The specialist cells of the immune system in our organs and bloodstream.
- The electrical connections of the nervous system.
The specialist cells are like the brain’s spy network. They communicate with the brain by means of the nervous system’s electrical connections. The brain, in turn, regulates the responses of the other various organs and systems within the body.
Groundbreaking Research
A few decades ago, the experimental research of Kevin Tracey led to a quantum leap in our understanding of the brain-pain connection.
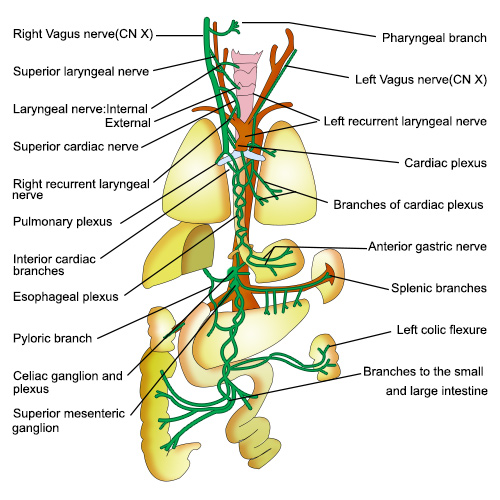
Tracey theorized that the brain might be using the nervous system in general – and the vagus nerve in particular – to tell other organs to move the inflammation switch to the off mode. Further research has confirmed that inflammation in body tissues is directly regulated by the brain. It tells the rest of the body when and where both to raise the temperature, and to lower it.
The vagus nerve is so-named because it’s like a wanderer, or vagrant, traversing its way through the upper body. The longest of the cranial nerves, it controls the parasympathetic nervous system (i.e., rest and digest) and connects the brain to the visceral organs. In other words, it tells the brain how the gut is feeling.
Tracey’s research led to a remarkable conclusion: vagus nerve stimulation via electrical stimulus effectively blocks inflammation. With that, a new applied science was born.
Bioelectronics and Vagus Nerve Stimulation: A Promising New Approach to Inflammation
Vagus nerve stimulation is at the heart of bioelectronics, a field of medicine that harnesses and applies electrical energy to reduce inflammation, or even to eliminate it altogether.
Bioelectronics has two ways of doing this:
- Implantation surgery (costly and invasive)
- Microcurrent therapy (affordable and non-invasive)
Even rheumatoid arthritis, a crippling condition for which conventional medicine offers no cure, responds to bioelectronic treatment. The potential life-changing implications are myriad!
Click this link to learn more about these exciting developments and how you and your loved ones can benefit from them. Our free special report, Inflammation: The Hidden Source of Chronic Pain, is available here. In it, you’ll learn specifically about:
- The inflammation-pain connection
- The root of all autoimmune disorders
- The link between mental health and inflammation
And so much more!
Ready to learn more?
If you’d like to learn how you could do non-invasive Vagus Nerve Stimulation safely from the comfort of your home, book a complimentary phone consultation here at PainFreeConsult.com or call us toll-free at 1-888-758-0851 and speak to a member of our expert team.